Ehmet Health is a privately held, emerging medical device company with an innovative device for providing radiation as a treatment for breast cancer. Radiation therapy remains a mainstay of treatment for breast cancer; although, right now many cancer patients are seeing significant disruption to their care due to COVID-19. No doubt, this is not the last time we will see this problem. Cancer patients and the doctors that treat them need better options, and Ehmet's MammoKnife is exactly what is required.
COVID-19's Impact on Cancer Care
The shutdown of the U.S. economy and national "stay-at-home" orders resulting from the ongoing SARS-CoV-2 (coronavirus) pandemic is clearly having a detrimental impact on both businesses and individuals. The effect can be seen at restaurants and shopping centers and in the significant spike in the U.S. unemployment rate as businesses close their doors until an “all-clear” sounds. However, what may not be as obvious is the impact on cancer patients.
COVID-19 is putting a substantial strain on the healthcare system in almost every major city in the United States and abroad. As a result, cancer patients are being triaged and care is being delayed for many seeking treatment, including push-backs in surgery, transplants, and radiation therapy (ASCO, April 2020). This obviously creates a significant risk for cancer patients, as a delay in treatment for any patient whether a slow or rapidly progressing or potentially curable tumors may outweigh the risks of COVID-19 exposure/infection; however, a retrospective analysis of cancer patients conducted in Wuhan, China between January and February 2020 shows a devasting effect on outcomes with COVID-19 co-infection. In a paper by Zhang et al in Annals of Oncology (in press, 2020), a strong association between anti-cancer therapy in the past 14 days and severe effects of COVID-19 infection was reported (HR=4.079, 95%CI 1.086-15.322, P=0.037) in 28 patients.
Patients Are Staying Home
Because of the imposing health concerns, many cancer patients are simply avoiding hospitals altogether, as these are the epicenters of COVID-19 disease. An article published in The Lancet Oncology on April 20, 2020 states, “The pandemic has meant a transformation of every aspect of cancer care” and that, “efforts are underway to relocate cancer teams and services away from general hospitals caring for patients with COVID-19 as much as possible” (Mayor S, 2020).
For breast cancer patients undergoing radiation therapy, the American Society of Breast Surgeons has established a triage system prioritizing only those with an immediately life-threatening and clinically unstable disease (Dietz et al, 2020). While the data suggest a short-term delay in radiation treatment in patients with a non-critical or stable disease does not have a material impact on outcomes, delays longer than eight weeks can result in an increase in recurrence (Huang et al, 2003). The first "stay-at-home" guidelines from the White House came in mid-March 2020. No doubt this caused significant anxiety for cancer patients, most of whom are already in a vulnerable emotional state, by putting off treatment since the U.S. coronavirus outbreak began.
The ensuing lack of patients undergoing cancer treatment is also having a material impact on the financial health of hospitals. Radiation bunkers are incredibly expensive to build and maintain. It might cost between $3 and $5 million to build shielded bunkers and another $5 million to equip the facility. A radiation oncology department needs patients to run the business and if patients are staying home, departments can become cash-strapped rather quickly. COVID-19 is compounding an issue of financial unsustainability already seen in many rural hospitals around the U.S.
An analysis conducted in February 2020 by Chartis Center for Rural Health identified over 450 rural hospitals on the brink of closure before the COVID-19 pandemic, with nearly half identified as "most vulnerable" to closing due to a myriad of political, structural, and socio-economic issues. A separate analysis by Guidehouse in March 2020 concluded that one out of four rural hospitals in the U.S. is at risk of closure due to significant financial distress, and similarly, this analysis was conducted before COVID-19 shut down most of the country in a seemingly strong U.S. economic environment. Where will these patients be treated?
For Rural Hospitals, The Situation is Dire
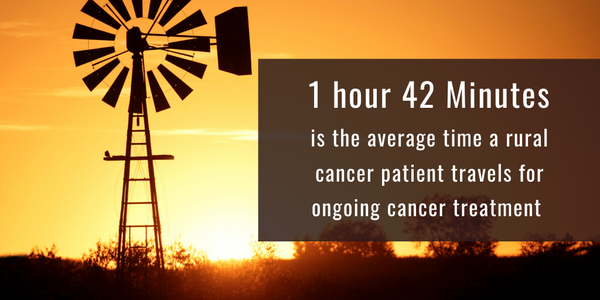
The situation is particularly dire in the South and Midwest. States like Tennessee, Mississippi, Alabama, Arkansas, Nebraska, Wisconsin, Wyoming, and Oklahoma have large rural populations with community-based hospitals. A study in Iowa found that 50% of cancer patients travel more than 30 minutes to receive treatment, and some patients in most rural areas end up traveling three-times as long. As noted above, radiation oncology bunkers are extraordinarily expensive to build and maintain. As a result, over 90% of cancer radiation is done at major cancer centers or academic hospitals also found near large cities. Travel to these areas from rural America creates financial hardship and results in significant emotional stress for patients. This is a major reason why survival rates and outcomes are worse in low-income areas inside the U.S., and abysmally low in under-developed regions outside the U.S. There were significant logistical and financial challenges to rural cancer care in the U.S. before COVID-19; today the situation is worse.
This is an important issue because radiation therapy remains a mainstay of treatment for breast cancer patients. In fact, about 60% of all breast cancer patients will have radiation at some point during their treatment. Yet rural hospitals face significant challenges in providing patients safe, convenient, and cost-effective care. And today, because of COVID-19 and its impact on major cities like New York City, even the largest medical centers are seeing patients stay home.
MammoKnife Comes to You
Ehmet’s MammoKnife was designed to address many of these challenges noted above to rural cancer care in the U.S., and provides the most needed solution large medical centers are looking for in the face of future infectious disease pandemics or even natural disasters like hurricane Sandy, Katrina, or Harvey that shut down major metropolitan areas for extended periods of time.
MammoKnife is the first self-shielded 6-MV linear accelerator designed specifically to treat breast cancer patients with the current standard-of-care for both whole or partial breast irradiation. Its design lends itself to even the emerging and novel radiation therapy techniques. Self-Shielded means the radiation treatment does not need to be restricted to a radiation bunker. In fact, MammoKnife has been designed for deployment on a standard trailer (view 3D animation) allowing for a first of its kind platform delivering precision therapy in a mobile setting. The turn-key system is designed to be deployed to any urban or rural location by partnering with community medicine and outpatient centers.

Instead of getting the patient to the hospital, the hospital can come to them. A machine that is self-shielding can be used outside of a traditional radiation bunker. This could save a rural hospital millions of dollars and make it so that more patients have access to treatment. If that machine is specifically built for breast cancer applications, advanced treatment plans can be used that result in less skin damage on the outside, and patients can be positioned properly to minimize systemic spill-over to nearby organs on the inside. Clinical data show that accelerated partial breast irradiation is non-inferior to whole breast irradiation in terms of long-term outcomes, but many women still choose whole breast irradiation because it results in less cosmetic damage and the eventual need for reconstructive surgery.
A shift in radiation oncology treatment for breast cancer has been towards hypofractionation. Hypofractionated radiation therapy is a type of radiation therapy where a higher dose of radiation is administered over a shorter timeframe. Up until recently, the effectiveness and cosmesis of hypofractionated radiation therapy had limited long term data that had been published for breast cancer. However, randomized clinical trials proved that this therapy is comparable to other radiation therapies in effectiveness while being less toxic (Gilibo et al, 2018). The challenge for hypofractionation, however, is patient access. Treatment might be for five days over a week-and-a-half. For rural Americans living hours away from the largest medical center in their state, the expense of travel and hotels, etc... might be too great.
With MammoKnife, a large medical center like MD Anderson, Penn Medicine, Karmanos, or Roswell Park can set up satellite treatment locations, partnering or co-branding the service with local community hospitals, and vastly increase access to care. Additionally, as reimbursement in the U.S. moves to the Bundled Payment or Alternative Payment Model (APM), much as it is in almost all areas outside the U.S., hospital administrators are going to have to figure out how to provide a cost-effective solution while delivering the same high-quality care to patients. MammoKnife addresses the issue of value-based care and payment bundling by delivering efficacious levels of treatment in a far more efficient protocol.
A Significant Market Opportunity
With 268,000 new cases of breast cancer in the U.S. each year and another 400,000 in Europe, the breast cancer radiation market represents an enormous market opportunity. Ehmet has an opportunity to not only sell the MammoKnife device to large medical centers in urban areas looking to expand their breast cancer radiation business but also tackle the wide-open rural market through mobile platforms and turn-key solutions. Surgery centers, breast cancer clinics, or even places like Walmarts and Amazon that have recently entered the world of healthcare, can offer a precision therapy that’s closer to the patient, simple to use, and profitable. It is clear that COVID-19 is having a material impact on cancer patients. People are staying home and delaying potentially life-saving treatments. During Hurricane Katrina and Sandy, hospitals closed and many saw disruption in the availability of care. Ehmet's mobile treatment centers have the potential to be a real game-changer in these situations. It’s even a particularly attractive opportunity for emerging markets.
At approximately $2.5 million per unit, with only 10% market penetration in the U.S. and Europe, the MammoKnife will be a multi-billion dollar product opportunity. The revenue line will incorporate annuity-like revenues from service contracts, which will price 8-10% of the unit sales price and run for a decade after placement. MammoKnife is being developed under the FDA’s 510(k) regulatory pathway because the device has “substantial equivalence” to existing machines. The U.S. 510(k) pathway does not require clinical trials prior to approval. Moreover, reimbursement codes in the U.S. for the therapies delivered by the machine are already in place and the first customers have been identified. This greatly simplifies the path to market and removes significant risk and cost of commercialization. The pathway in Europe is similar, which presents a tremendous opportunity for Ehmet and MammoKnife, the emerging markets only add to the potential.